kericure wound care clinical evidence
FOR BEST RESULTS, USE OUR KERICLEANZ ANTISEPTIC SPRAY TO CLEAN AND DISINFECT BEFORE APPLYING ANY OF OUR ADVANCED WOUND DRESSINGS
Partial Thickness Burn managed in military training environment with Field Shield
Authors: Rick Hammesfahr, MD – Tactical Medical Consulting, Georgia, USA; Kerriann Greenhalgh, PhD, KeriCure Medical, Tampa, FL, USA
Background
Traumatic injuries are common in both civilian accidents and military operations. When inadequately managed, superficial wounds may progress to cellulitis, abscess, or sepsis, contributing to lost duty time, hospitalization, increased consumption of antibiotics and dressings and reduction in operational capability. Ignoring relatively minor wounds in operational areas that have limited hygiene, adverse environmental conditions, limited medical supplies, and limited evacuation capability results in an increased probability of infection development. Early application of advanced dressings that are simple to use, portable, and provide both antimicrobial coverage and pain control could mitigate these risks, thus decreasing medical resupply needs, development of cellulitis and infections, and the subsequent need for medical evacuation.
Methods
This prospective observational study was conducted following written informed consent. A 26-year-old male presented with a partial-thickness thermal burn to the thoracic region of the back secondary to contact with an ejected brass cartridge. The injury was managed on an outpatient basis by the subject’s battalion medic. Upon notification, the wound was cleansed with KeriCleanz® Antiseptic Spray, a topical wound cleanser containing a small amount of hydrogen peroxide (1%) and silver hydrosol antimicrobials. Field Shield was subsequently applied directly to the cleansed wound surface. Neither product was rinsed or removed following application. The treatment was well tolerated, with no reported adverse effects or complications.
The Field Shield dressing was spray applied daily (2 to 3 sprays per dressing application) for 5 consecutive days, then applied 2 additional times prior to reaching 100% epithelialization by Day 14 post-injury. No removal of the dressing was required between applications, and the subject maintained routine hygiene and showering throughout treatment. Subject continued their training exercise and routine activity, including aquatic training, ruck runs, and other physical activities.
Results
Field Shield Wound Dressing demonstrated effective, rapid, and durable wound management in the presented case. No evidence of infection or complications was observed throughout the healing process. By day 14, the wound exhibited smooth epithelial margins with no visible scar formation. The subject reported an absence of pain or discomfort at the wound site during the course of recovery.
Conclusions
KeriCure Medical’s Field Shield® Wound Dressing demonstrated rapid wound closure, effective infection prevention, pain mitigation, and enabled the Service Member to maintain full duty status throughout treatment. The product’s practical advantages included ease of application, complete coverage and protection of high-friction areas, transparency to facilitate continuous wound assessment, and reduced need for additional dressing materials during burn management. The dressing’s durability and waterproof properties permitted uninterrupted participation in training exercises during the healing process. Its compact, multi-use design and minimal training requirements highlight its potential value for deployment in military and other resource-limited or austere care environments.
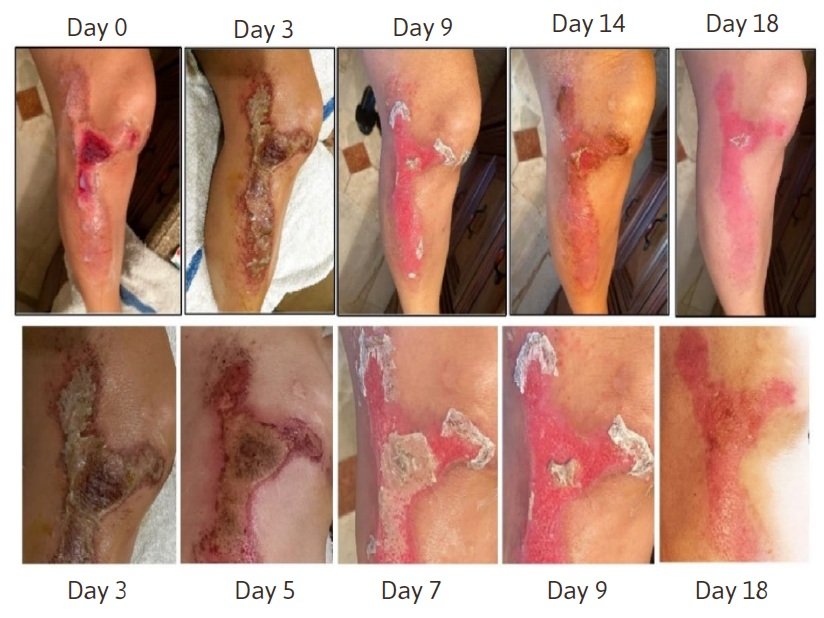
DEEP PARTIAL THICKNESS FRICTION BURN TREATED WITH ADVANCED SHIELD SILVER WOUND DRESSING
Authors: Ronald Scott, MD, Founder and Medical Director, The Wound Care Clinics of North Texas, Plano, TX, USA; Kerriann Greenhalgh, PhD, CEO and CSO, KeriCure Medical, Wesley Chapel, FL, USA
Background
Point-of-Injury treatment of large area burn and abrasion wounds is critical to rapid recovery and maintaining readiness. A single case study is presented here of large surface area, deep partial thickness burn and abrasions, where a combination treatment plan using two novel wound dressings was implemented at point-of-injury throughout continuum of care. KeriCure Medical’s Advanced Seal plus Pain Relief barrier (AS Pain) and Advanced Shield Hydrogel Wound Barrier (ASWB) were assessed for infection mitigation, healing, pain management and autolytic debridement capabilities.
Methods
Patient was clinically assessed and prescribed a treatment regimen of two KeriCure Medical products as the primary wound dressings. AS Pain containing 2% lidocaine was prescribed as the primary dressing for pain management and infection control, adding ASWB from Day 2 to 7 for added moisturization and infection control, as well as superior management of wound exudates. ASWB was preferred by the patient, noting the soothing nature of the thicker hydrogel calming the friction burn, and was continued by the patient as the sole dressing after Day 7. The patient documented wound progress throughout the treatment regimen, as well as participated in two independent wound assessments and a final wound assessment approximately four months after initial injury. Various secondary dressings were trialed by the patient, with Telfa being the favored secondary dressing when used with ASWB.
Results
Each wound area had remarkable healing, with complete closure and re-epithelialization by Day 21 for the deep partial thickness burn wound, and by Day 10 and 11 for the upper thigh and inner elbow abrasions, respectively. Wound cleaning and mechanical debridement was aided by the moisturization benefits of ASWB hydrogel, allowing eschar to easily slough off. Surgical debridement was avoided with the use of the wound dressing combination, aiding autolytic debridement of necrotic tissue central to the burn wound. Cosmetic outcomes were favorable, with no visible scarring and only slight discoloration remaining at the final follow up visit. No signs of infection were noted throughout healing.
Conclusions
Point-of-injury treatment with two novel wound dressings provided improved healing outcomes, simple dressing change regimen, local pain management and infection prevention. Self-application and elimination of surgical debridement allowed for a shortened recovery period.
Improved Wound Healing Outcomes for Large Surface Area Burn Wounds with a Novel Spray on Antimicrobial Wound Dressing
Authors: Kerriann Greenhalgh, Marc Thompson, Robert Christy
Background
The purpose of this study was to evaluate two versions of KeriCure Medical’s Field Shield Wound Dressing (FSWD) to support wound healing and mitigate infection in a large TBSA porcine burn wound model. It investigated the ability of the Field Shield dressings to facilitate wound healing in the form of wound closure, to aid autolytic debridement and improve wound healing outcomes following a prolonged field care treatment regimen followed by the standard of care.
Methods
It was anticipated that the FSWD products may improve wound healing outcomes in the form of wound closure as compared to the SOC dressings. The primary endpoint of the study was wound closure. Secondary healing outcomes monitored in the study included burn progression, necrotic tissue management, granulation tissue, local edema and erythema. Re-epithelialization, depth of wound necrosis, granulation and collagen tissue deposition were assessed histologically using hematoxylin & eosin (H&E) staining as the primary IHC metric.
Results
Field Shield Wound Dressing products supported healing of the large surface area, deep partial thickness burn wounds over the 35 day study similarly to the control dressings (gauze and Silverlon). Field Shield demonstrated a higher propensity for burn wound closure (as measured by burn wound surface area) when compared to Silverlon and gauze, indicating substantially equivalent effectiveness in managing larger size burn wounds, a challenging burn model.
While not an endpoint of this study, it was noted by the study team that the Field Shield managed burn wounds were cleaner wounds, with a lower severity of exudate in terms of gross observations of volume, and that the device aided autolytic debridement with necrotic sloughing observed prior to surgical debridement and easier removal of necrotic tissue and during dressing changes than Silverlon and gauze controls throughout the study.
A marked reduction in erythema (redness) was observed upon application of the Field Shield dressings, with rapid improvement and calming of inflammation within minutes of application to the burn. The study team also noted via gross observations that there was significantly less necrosis and edema on Day 21 and 35 than the control devices, with visible reduction in inflammation and redness observed upon application of the Field Shield devices, indicating lower pain levels and inflammation may be associated with dressing change for the Field Shield device.
There were no instances of marked infection in any of the wounds, with minimal or no bacterial contamination observed in nearly all wounds throughout the study histologically. These findings support the secondary aim of the study, confirming the ability of the Field Shield dressings in mitigating infection development for the burn wounds.
Conclusions
With >50% wound closure for FSWD treatments, the data supports use of FSWD at near point-of-injury can reduce healing times, mitigate infection development and burn expansion, and provide a simple, easy to use solution in acute care and beyond.
Wound Repair and Regen. Volume31, Issue2, March/April 2023, Concurrent Oral Presentations, Burns (P1).
Field shield Wound Dressing Promotes Healing and Reduces S. aureus Infection in a Prolonged Field Care Treatment Regimen In Vivo for Full Thickness Burn Wounds
Authors: Ronald Scott, MD; Kerriann Greenhalgh, PhD
Background
Infection of traumatic wounds carries a life-threatening risk and can promote severe morbidity including sepsis, amputation, prolonged hospital stays, disfigurement/scarring and years of battling chronic infections. Combat related wounds are especially at risk of infection where dirt and debris embed wounds, initiating an infection within 66 minutes of injury. With the golden hour anticipated to extend to a Golden day, management of traumatic wounds in far forward and prolonged field care is critical to preventing co-morbidities and promoting wound healing. KeriCure Medical’s Field Shield Wound Dressing (FSWD) is an innovative solution for treatment of large surface area burn wounds and combat wounds at point-of-injury throughout the continuum of care. This pilot preclinical study investigated the ability of the spray on dressing containing a potent silver hydrosol (antimicrobial) and lidocaine (anesthetic) to act as an effective treatment for infected, full thickness burn wounds following a prolonged field care regimen in comparison with a standard of care silver dressing (Silverlon).
Methods
A total of 16 full thickness burns (8 per pig) were created using a thermally heated block, then 4 sites per animal were treated with Field Shield and 4 sites per animal were dressed with Silverlon. Silverlon had additional treatments applied (saline soaked gauze, Tegaderm), then all sites were wrapped with secondary dressings and left untouched for 72 hours (with the exception of gentle swabbing on Day 2 for microbial burden assessment). Wounds were again swabbed then surgically debrided on Day 4 (72 hours post-burn) before reapplying the dressings. Dressing changes followed standard Role 4 protocol thereafter thru Day 10, with assessments continuing until Day 28 (final). Histology samples were taken on Day 7, 14 and 28.
Results
Field Shield® Wound Dressing supported healing in management of full thickness burn wounds infected with S. aureus, with noteworthy areas of superior performance to Silverlon. FSWD demonstrated superior antimicrobial activity on the burn wounds with a single application on Day 1 as compared to Silverlon. FSWD also demonstrated stronger antibacterial activity in the prolonged field care timeframe, where no CFUs or significantly reduced CFUs (log 2 reduction) were measured by Day 4. Silverlon sites measured an increase in CFUs or a slight reduction (log 1) during the PFC period, presumably due to a lack of moisture necessary for the silver activation in Silverlon.
Wound size measurements suggest that FSWD may prevent burn progression in PFC, where no change was observed for FSWD from Day 2 to Day 4, compared to a 4% increase in wound size for Silverlon sites. Wound size measurements for FSWD showed an overall smaller wound by Day 28 than the Silverlon burn sites.
No exudates were observed after Day 10 for FSWD, revealing a cleaner wound site and better moisture balance to support healing. Visual observations showed comparable re-epithelialization and granulation scores. Histopathology evaluation showed that wound healing process overall was similar for both treatments. FSWD sites showed slightly lower granulation scores on Day 28 compared to Silverlon, but had comparable re-epithelialization and collagen scores, with slightly lower necrotic tissue scores than Silverlon.
Conclusions
Overall, the KeriCure Medical® Field Shield® Wound Dressing supported healing of full-thickness burn wounds infected with S. aureus over the 28-day study, with superior performance to Silverlon during the prolonged field care timeframe. This suggests that FSWD is a potentially viable treatment option for full thickness burn wounds at point-of-injury through the continuum of care.
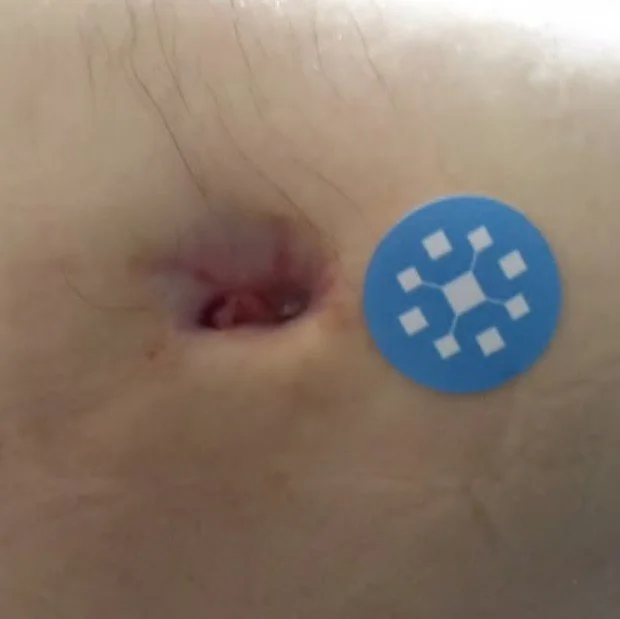
Abdominal Moisture Associated Skin Damage with Draining Fistula
Patient Specifics: 56 year old, Male
Injury/Condition: Moisture associated skin damage (MASD) with draining fistula of the abdomen.
Treatment: Advanced Shield MAX Silver Wound Barrier was applied directly to the wound after cleansing, then covered with a non-stick absorbent pad as the secondary dressing. Monthly dressing change consisted of reapplying the Advanced Shield Max Wound Barrier with a fresh pad as secondary dressing for exudate management.
Outcome: Exudate management was achieved with the combination of Advanced Shield MAX and the absorbent pad, allowing the skin to heal over the six month period. Inflammation was markedly reduced after the first application of Advanced Shield MAX. Edema reduction was achieved with the treatment.
Summary: Use of Advanced Shield MAX provided an effective barrier over the abdominal skin, mitigating further deterioration and damage from moisture. The combination of Advanced Shield MAX with an absorbent pad achieved complete healing within six months of treatment.
Large Non-Healing Stage IV Pressure Injury to Sacrum
Patient Specifics: 72 year old, Female
Injury/Condition: Stage IV pressure injury to sacrum with moderate exudate and peri-wound ulceration and biofilm Advanced Seal plus Pain Relief was applied to peri-wound skin for inflammation management, to prevent wound expansion, and support healing of the Stage II pressure injuries that developed around the main pressure wound.
Treatment: KeriCleanz was applied directly to the wound and sprayed onto sterile gauze that was applied as primary dressing. A super absorbent foam dressing was applied as secondary dressing.
Outcome: The non-healing pressure injury saw significant improvement with the onset of this multi-treatment approach. The established biofilm was eradicated from the wound bed, allowing the wound to begin healing. Peri-wound skin saw early healing, allowing for PI wound closure within 4 months of treatment, without debridement.
Summary: A large, non-healing Stage IV pressure injury was effectively managed with a combination of the KeriCleanz antiseptic wound cleanser spray, Advanced Seal plus Pain Relief for peri-wound management, and a super absorbent foam dressing. Peri-wound skin saw significant reduction in erythema and closure of the Stage I PI quickly. Complete granulation was achieved by 4 months of management, with epithelialization reaching > 75%.
Mid Lateral Left Thigh Unstageable Pressure Injury with Biofilm
PATIENT: 68 year old, Male
INJURY/CONDITION: Unstageable pressure injury (16.8cm2) at left trochanter at midlateral left thigh with established biofilm and peri-wound erythema. Wound edges clearly outlined. Moderate exudate.
TREATMENT: KeriCleanz Antiseptic wound cleanser was applied to the wound with a super absorber dressing applied on top of the wound as the over dressing for exudate management. Bedside (non-surgical) debridement was performed 12.26.2021 and 2.3.2022.
OUTCOME: By 60 days, no signs of infection remained, and the wound showed significant granulation (>75%). Wound reached 75 - 100% epithelialization by 3 months of treatment. No surgical intervention was required for healing.